Every tuberculosis patient gets free drugs under the government’s Revised National Tuberculosis Control Programme (RNTCP). However, the patients frequently discontinue them because of the extreme side-effects they suffer, including that of psychological disorders
Rekha Kishan Shinde says she is lucky to be alive. This 35-year-old from Sarola village, Latur, first fell ill with typhoid, followed by malaria, followed by a bout of pneumonia. With her weight down to a measly 30 kilos, and an immune system already battered by the consecutive illnesses, she was an easy target for multi-drug resistant (MDR) tuberculosis.
Not surprisingly, all of this happened to her in Mumbai, one of the epicentres of TB in India.
“My husband works in Mumbai as a driver and I went to live with him in Bhiwandi for three years. After the first year I kept falling ill,” she said.
Like so many other migrant families in India’s commercial capital, Rekha and her husband lived in a Bhiwandi slum, a two-room house outside which open gutters bubble past that they share with five others. If there ever was the perfect conditions for contracting TB, this was it.
When medicines taken from a local doctor had no effect, Rekha’s husband sent her back to Sarola, where her two young daughters live, so that she could get better.
Rekha’s decision is typical. Like her, a majority of TB patients first head to their local doctor when the coughing becomes persistent and they start to lose weight. The doctor will prescribe antibiotics and send them home. The symptoms will return. Unaware, the patients will continue to spread the infection, making India a hotbed of the disease.
Never a first choice
This year, the World Health Organisation (WHO) revised the number of TB patients in the world to 10.4 million and those in India to 2.8 million cases from the earlier estimate of 2.2.
According to WHO figures for 2016, India has 79,000 MDR-TB patients out of a global total of 5,80,000, making it home to roughly one in every six drug-resistant TB patients in the world.
Under the government’s Revised National Tuberculosis Control Programme (RNTCP), medicines for TB are given free of cost and yet, according to government’s own estimate, almost half the patients – including the poorest of poor – choose the private sector.
Why?
Shafiya’s village has a primary healthcare centre but it is open for barely a few hours each day. The family lives in Latur’s Rui village. The doctor is more often than not absent from the clinic, leaving inexperienced nurses to administer injections and basic treatment.
Not surprisingly then, in spite of their abject poverty, when the disease struck, Rabiya’s family turned to private practitioners.
“Poor patients eventually come back to the government system once they run out of money, but they almost always go to the private sector first,” said Ganesh Patil, a coordinator in Maharashtra for the not-for-profit organisation PSI that works with TB patients.
Shinde, for example, was introduced to the government’s TB programme by an NGO worker but according to WHO, 41 per cent of TB patients slip through the gaps. They never receive any care and are rarely diagnosed in time.
An August 2016 report in the medical journal Lancet claimed that almost a third of TB patients in India, or about 2.2 million, are treated in the private sector alone. The total number of TB patients in India, by that estimate, could be as high as 6.8 million, more than twice the revised WHO estimates. Members heading the RNTCP, India’s TB programme, were part of the study that took into account the sale of drugs in the country to estimate the number of patients.

The ‘jhol-jhal’ doctors
In the tribal areas of Melghat, the lack of trust in the publicly-funded health sector leads to disastrous consequences. The first option is always a ‘spiritual healer’ that are dismissively called ‘jhol-jhal doctors’ by others.
Patients often pay with their lives.
What is most worrying to health practitioners, though, is that in rural India private practitioners often tend to be, at best, doctors with dubious degrees or, at worst, none at all. The medicines prescribed have no uniformity and are not in line with either the DOTS programme or WHO guidelines.
“Private practitioners prescribe high doses of antibiotics. This masks TB symptoms like cough for sometime but builds drug resistance in patients,” said Dr Sachin Mhaske, a Latur-based AYUSH practitioner.
The government is working with many such private AYUSH practitioners like Mhaske, trying to coopt them into following prescribed guidelines and become DOTS providers themselves. It is an uphill task.
“Private doctors have to notify the government about the TB cases but many don’t do so. A TB patient guarantees regular income for months that doctors don’t want to lose,” added Dr Mhaske. Most patients never find out that the medicines responsible for their debt are available free of cost at a government health centre.
Deadly side-effects
As with most modern allopathic medicines, the anti-TB drugs under the DOTS programme also come with severe side-effects, another leading cause of patients turning away from the treatment regimen midway. Once they stop taking the medicines, they become infectious and put others around them at danger.
The medicines under the DOTS programme, which follows WHO guidelines, are toxic and the side-effects are often too much to bear for the body of an under-nourished migrant worker in rural India. Worse, the dosage is the same for a person weighing anywhere between 30 kg and 60 kg – often with disastrous consequences.
The regime is gruelling and treatment duration can range from six months to as many as five years depending on the strain of TB a patient has.
Over that period, a patient is required to take as many as seven tablets every alternate day. Nausea, mild hearing loss, and drowsiness are just some of the consequences; memory loss and long term and even insanity in some cases is a reality for most patients with MDR-TB.
“I couldn’t work for over six months and had to shut my shop,” he added.
Unable to work, debt piles up.
“Adverse drug reactions do substantially increase expenditure for the patient. They can lead patients to interrupt or abandon treatment, resulting in higher rates of treatment failure and acquired resistance, as well as an increase in the number of tuberculosis cases,” concedes Dr Om Prakash Bera, State Technical Consultant (TB), International Union Against TB and Lung Disease.
Unheard and invisible
Though both Bhosle and Shinde are TB free now, their illness has left them in considerable debt. But, if the medicines are free, what are the patients spending on?
“My weight was very low and I needed nutritional supplements that had to be bought from outside,” Shinde explains.
Sunil Bhosle, 31, TB surviver
Doctors often prescribe for nutritional supplements or drugs to counteract side-effects. While they are almost never available in tribal areas, even the larger district hospitals are often out of stock.
Private doctors, on the other hand, stick to the daily regime, are flexible with the dosage and, most importantly, hear the patient out.
“Our TB programme is focussed on the disease and not the patient. It is a disease that is associated with poverty and perpetuates poverty,” says Dr Anurag Bhargava of Jan Swasthya Sahyog (JSS) that runs low-cost health programmes in rural Chhattisgarh.
Those part of the RNTCP programme often work in silos and the effort is to ensure that the patient does not end on the defaulter list. A patient’s concerns are rarely the programme’s problems.
Rabia Sheikh (19), lived with her husband, in-laws and brother-in-law in a two-room house in Mumbai’s Bhandup area. When a local doctor suspected TB, her husband sent her to Latur, but the five-months pregnant teenager is concerned how the medicines will effect her unborn child.
“I am going to a private doctor, spending around Rs 2,000 a month on my medicines,” she says.
A change in dosage requires permission from a doctor who is often at the district hospital which itself is often as much as 100 kms from a remote village.
For most TB patients the road to recovery is a lonely one. A little hope would go a long way in the recovery process but, unfortunately, there is no one to lend them an patient ear.
(The final part of this three-part weekly series will explore the human face of the disease and examine the toll it takes on families. The author is a recipient of the 2016 REACH Lilly MDR-TB Partnership National Media Fellowship for Reporting on TB.)
![submenu-img]() Meet Gautam Adani’s ‘right hand’, used to work as teacher, he’s now Rs 1600000 crore…
Meet Gautam Adani’s ‘right hand’, used to work as teacher, he’s now Rs 1600000 crore…![submenu-img]() Meet actor who worked with Amitabh Bachchan, Aishwarya Rai, entered films because of a bus conductor, is now India's..
Meet actor who worked with Amitabh Bachchan, Aishwarya Rai, entered films because of a bus conductor, is now India's..![submenu-img]() Meet Bollywood star, who was a tourist guide, married 4 times, went bankrupt, his son died by suicide, then...
Meet Bollywood star, who was a tourist guide, married 4 times, went bankrupt, his son died by suicide, then...![submenu-img]() This actor made Sharmila Tagore forget her lines, once did film for Rs 100, could never be a superstar because..
This actor made Sharmila Tagore forget her lines, once did film for Rs 100, could never be a superstar because..![submenu-img]() Volkswagen Taigun GT Line, Taigun GT Plus launched in India, price starts at Rs 14.08 lakh
Volkswagen Taigun GT Line, Taigun GT Plus launched in India, price starts at Rs 14.08 lakh![submenu-img]() DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'
DNA Verified: Is CAA an anti-Muslim law? Centre terms news report as 'misleading'![submenu-img]() DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message
DNA Verified: Lok Sabha Elections 2024 to be held on April 19? Know truth behind viral message![submenu-img]() DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here
DNA Verified: Modi govt giving students free laptops under 'One Student One Laptop' scheme? Know truth here![submenu-img]() DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar
DNA Verified: Shah Rukh Khan denies reports of his role in release of India's naval officers from Qatar![submenu-img]() DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth
DNA Verified: Is govt providing Rs 1.6 lakh benefit to girls under PM Ladli Laxmi Yojana? Know truth![submenu-img]() Remember Abhishek Sharma? Hrithik Roshan's brother from Kaho Naa Pyaar Hai has become TV star, is married to..
Remember Abhishek Sharma? Hrithik Roshan's brother from Kaho Naa Pyaar Hai has become TV star, is married to..![submenu-img]() Remember Ali Haji? Aamir Khan, Kajol's son in Fanaa, who is now director, writer; here's how charming he looks now
Remember Ali Haji? Aamir Khan, Kajol's son in Fanaa, who is now director, writer; here's how charming he looks now![submenu-img]() Remember Sana Saeed? SRK's daughter in Kuch Kuch Hota Hai, here's how she looks after 26 years, she's dating..
Remember Sana Saeed? SRK's daughter in Kuch Kuch Hota Hai, here's how she looks after 26 years, she's dating..![submenu-img]() In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding
In pics: Rajinikanth, Kamal Haasan, Mani Ratnam, Suriya attend S Shankar's daughter Aishwarya's star-studded wedding![submenu-img]() In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month
In pics: Sanya Malhotra attends opening of school for neurodivergent individuals to mark World Autism Month![submenu-img]() DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?
DNA Explainer: What is cloud seeding which is blamed for wreaking havoc in Dubai?![submenu-img]() DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?
DNA Explainer: What is Israel's Arrow-3 defence system used to intercept Iran's missile attack?![submenu-img]() DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence
DNA Explainer: How Iranian projectiles failed to breach iron-clad Israeli air defence![submenu-img]() DNA Explainer: What is India's stand amid Iran-Israel conflict?
DNA Explainer: What is India's stand amid Iran-Israel conflict?![submenu-img]() DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles
DNA Explainer: Why Iran attacked Israel with hundreds of drones, missiles![submenu-img]() Meet actor who worked with Amitabh Bachchan, Aishwarya Rai, entered films because of a bus conductor, is now India's..
Meet actor who worked with Amitabh Bachchan, Aishwarya Rai, entered films because of a bus conductor, is now India's..![submenu-img]() Meet Bollywood star, who was a tourist guide, married 4 times, went bankrupt, his son died by suicide, then...
Meet Bollywood star, who was a tourist guide, married 4 times, went bankrupt, his son died by suicide, then...![submenu-img]() This actor made Sharmila Tagore forget her lines, once did film for Rs 100, could never be a superstar because..
This actor made Sharmila Tagore forget her lines, once did film for Rs 100, could never be a superstar because..![submenu-img]() Mumtaz urges to lift ban on Pakistani artistes in Bollywood: ‘Woh log hum logon se...'
Mumtaz urges to lift ban on Pakistani artistes in Bollywood: ‘Woh log hum logon se...'![submenu-img]() Not Kiara Advani, but this actress was first choice opposite Shahid Kapoor in Kabir Singh, she rejected because...
Not Kiara Advani, but this actress was first choice opposite Shahid Kapoor in Kabir Singh, she rejected because...![submenu-img]() IPL 2024: Yashasvi Jaiswal, Sandeep Sharma guide Rajasthan Royals to 9-wicket win over Mumbai Indians
IPL 2024: Yashasvi Jaiswal, Sandeep Sharma guide Rajasthan Royals to 9-wicket win over Mumbai Indians![submenu-img]() IPL 2024: How can RCB still qualify for playoffs after 1-run loss against KKR?
IPL 2024: How can RCB still qualify for playoffs after 1-run loss against KKR?![submenu-img]() CSK vs LSG, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report
CSK vs LSG, IPL 2024: Predicted playing XI, live streaming details, weather and pitch report![submenu-img]() RR vs MI: Yuzvendra Chahal scripts history, becomes first bowler to achieve this massive milestone in IPL
RR vs MI: Yuzvendra Chahal scripts history, becomes first bowler to achieve this massive milestone in IPL![submenu-img]() 'Yeh toh second tier ki bhi team nhi': Ramiz Raja slams Babar Azam and co. after 3rd T20I loss vs New Zealand
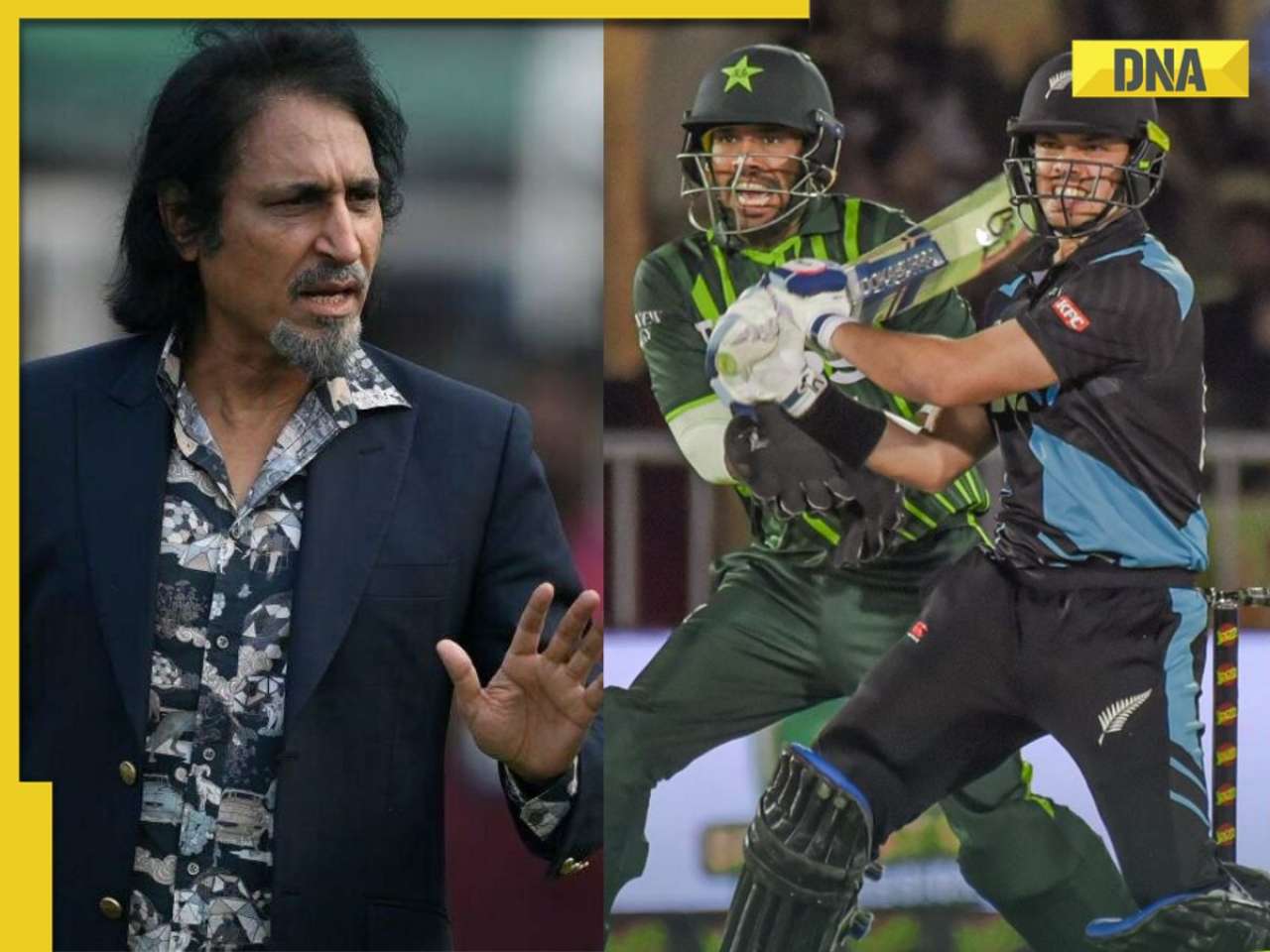
'Yeh toh second tier ki bhi team nhi': Ramiz Raja slams Babar Azam and co. after 3rd T20I loss vs New Zealand![submenu-img]() Mukesh Ambani's son Anant Ambani likely to get married to Radhika Merchant in July at…
Mukesh Ambani's son Anant Ambani likely to get married to Radhika Merchant in July at…![submenu-img]() India's most expensive wedding costs more than weddings of Isha Ambani, Akash Ambani, total money spent was...
India's most expensive wedding costs more than weddings of Isha Ambani, Akash Ambani, total money spent was...![submenu-img]() Meet Indian genius who lost his father at 12, studied at Cambridge, took Rs 1 salary, he is called 'architect of...'
Meet Indian genius who lost his father at 12, studied at Cambridge, took Rs 1 salary, he is called 'architect of...'![submenu-img]() Earth Day 2024: Google Doodle features aerial photos of planet's natural beauty, biodiversity
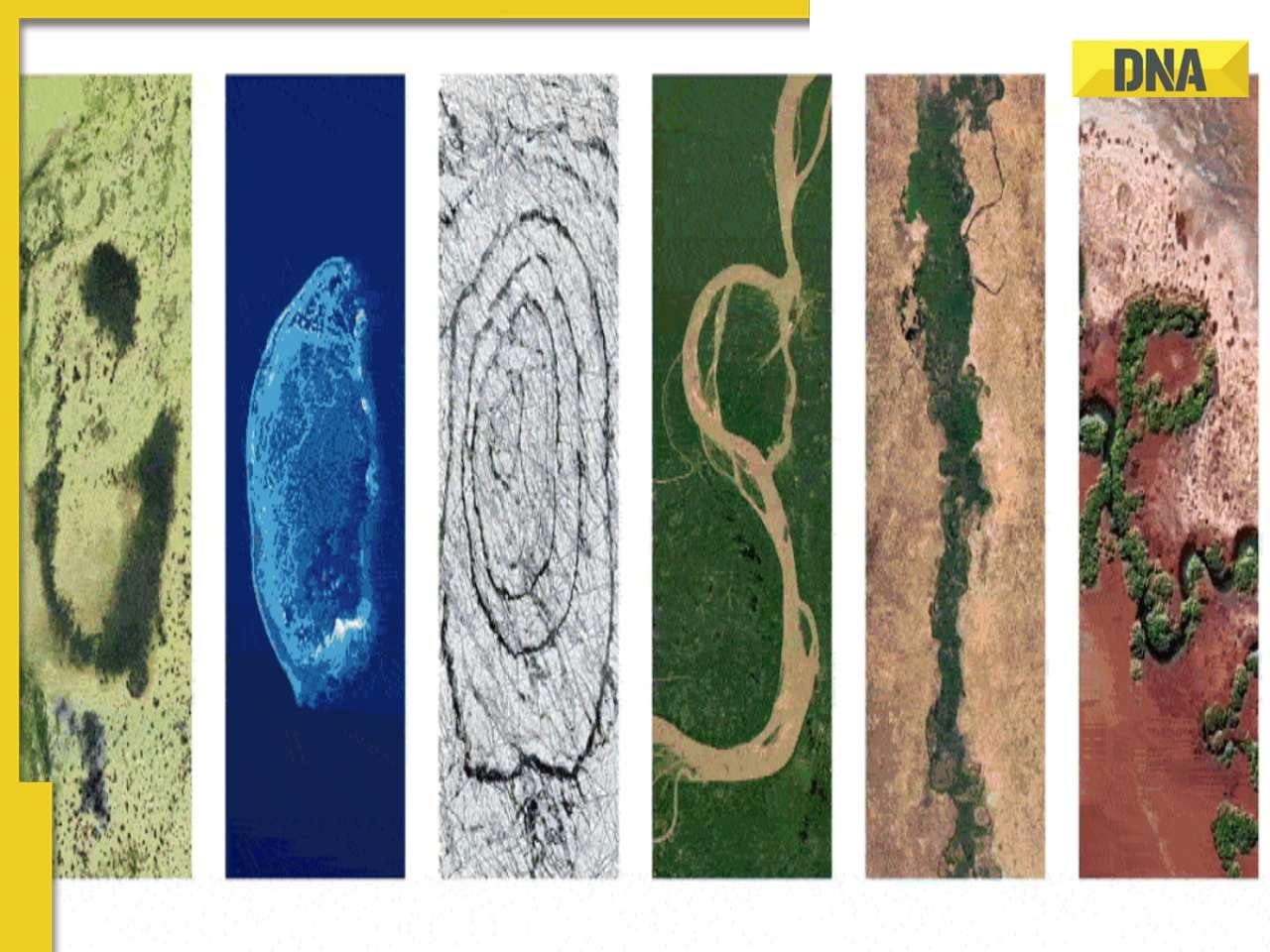
Earth Day 2024: Google Doodle features aerial photos of planet's natural beauty, biodiversity![submenu-img]() Meet India's first billionaire, much richer than Mukesh Ambani, Adani, Ratan Tata, but was called miser due to...
Meet India's first billionaire, much richer than Mukesh Ambani, Adani, Ratan Tata, but was called miser due to...


































)
)
)
)
)




)
)
)
)
)
)