Postural tachycardia syndrome (PoTS) is a form of dysautonomia, a term used to describe dysfunction of the autonomic nervous system. The condition can cause marked physical and cognitive impairment that can significantly impact upon activity. Although the exact UK prevalence is unknown, its frequency has stimulated an increase in studies. Occupational therapy services should place themselves in a position to respond to the potential need.
This study aimed to determine how PoTS impacts upon activity, in order for occupational therapists to understand the implications of this condition and develop appropriate interventions.
We recruited 201 adults (aged 18–70 years) via two patient support charities to participate in an online quantitative survey. Participants rated their experiences pre-symptoms versus present day in relation to their occupations, producing ordinal data under self-care, leisure and productivity domains, including their physical ability, motivation and fatigue levels.
The pre-symptom versus present day probability scores of <0.001 can be viewed as ‘very significant’ and confirm that PoTS has a significant negative impact across all three occupational domains.
In conclusion, PoTS has a significant negative impact upon occupation and is associated with considerable morbidity. With their understanding of the central role of occupation in wellbeing, occupational therapists may need to support people with PoTS in achieving a satisfying balance of occupations that will support their health.
Introduction
Postural tachycardia syndrome (PoTS) is a form of dysautonomia, a term used to describe dysfunction of the autonomic nervous system. Those living with PoTS can experience a vast array of symptoms that can be life-altering and debilitating.1 As well as a significant increase in heart rate upon standing, as a result of orthostatic intolerance, syncope and presyncope can occur, along with headaches, fatigue, palpitations, nausea and dizziness, which are usually relieved by lying down.2 Other autonomic functions, such as digestion, bladder control, temperature regulation and stress responses, may also be affected. Onset can be sudden or gradual, and for some individuals, there will be no known cause.1
The combination of physical and cognitive symptoms can significantly impact upon activity and, although the exact UK prevalence of this condition is unknown, there is an increased interest in the condition reflected in a greater frequency of studies within the literature. Therefore, occupational therapy services may anticipate additional opportunities to work with clients diagnosed with PoTS who experience mobility decline and disruption across employment, education and leisure pursuits.3 Occupational therapists recognise the purpose and power of these occupations and their role in health and wellbeing.4 Many researchers within the field have discussed the importance of individual choice and control over occupation in the lives of people who have been diagnosed with illness or impairment.5 Yerxa et al. state that “to engage in occupations is to take control”.6
The current published literature base primarily explores health-related quality of life,7,8 fatigue1 and cognitive function9 among those with a diagnosis of PoTS. However, information on the extent to which these factors impact upon activities of daily living remains sparse. Consequently, there was a need to carry out a UK-based, national quantitative investigation in order to gain a scoping view.
Methods
Our objective was to determine how PoTS impacts upon activity in order for occupational therapists to understand the implications of this condition and develop appropriate interventions.
We hypothesised that occupation will be affected by PoTS. This hypothesis was non-directional, as there is a lack of published literature to indicate a likely direction of the relationship between these two variables.
A web-based survey was selected to form the quantitative design of the study. This was hosted on Bristol Online Surveys for a period of 10 weeks and provided access to a national sample of individuals with a diagnosis of PoTS. Participants were recruited via two charity websites; STARS and PoTS UK.

The survey used demographic questions in order to learn more about the target population in conjunction with Likert scales. The Likert scales produced ordinal data under three clearly defined sections: self-care, leisure and productivity. Each scale was ranked 1–5 (1=low value, 5=high value), which allowed participants to rate their experiences pre-symptoms (PS) versus present day (PD) in relation to their day-to-day activities, including their physical ability, motivation and fatigue levels.
The theoretical heterarchy developed in Kielhofner’s Model of Human Occupation10 informed the development of the survey and acted as a body of knowledge to explore occupational impact.
Data analysis was performed within Statistical Packages for Social Sciences (SPSS) v23. The Wilcoxon signed-rank test located change within the sample by comparing PS versus PD.
Results
Participants
Formal data analysis took place on 201 adults including 194 women (96.6%) and seven men (3.4%). The age range of the sample was vast (18–70 years) with a mean age of 32.97 years. The mean age of first symptoms reported was 23.36 years with formal diagnosis being received at 30.35 years. The average period of time between first symptoms and diagnosis was found to be 6.99 years. There were 70 participants (34.5%) who were parents compared with 133 (65.5%) who were not. Employment status is shown in table 1.
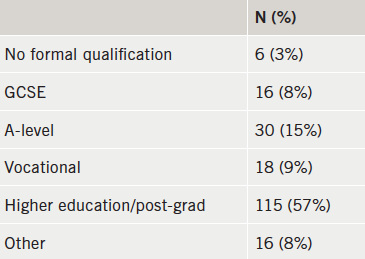
Table 2 displays responses to the following question: “What is the highest level of education you have completed? (If currently enrolled, please state the level you are working toward)”.
A focus on occupation: PS versus PD
The occupational variables explored were: motivation, performance capacity and fatigue. These were considered along with the occupational domains (table 3). The PS versus PD median scores provided a significance level of p≤0.001 across every Wilcoxon signed-rank test (table 4).



In addition to the self-care questions included in the study, participants were asked: “If you responded to the previous question with a number 4 or 5, do you have help to complete self-care activities from another person?” (table 5).
Discussion
Demographics
The mean age of participants in this study is 32.97 years, with 30.35 being the average age of diagnosis and this appears to be quite typical across the current literature base.1,7-9
This study has a sizeable sample and reports an excessive mean diagnosis delay of 6.99 years. This reflects a significant period of time that individuals are living with debilitating, often life-changing symptoms with no formal explanation of their cause. Within this period of time a significant proportion of this population are diagnosed with anxiety or panic disorder due to tachycardia and adrenaline sensitivity.11 However, research has shown that those with PoTS are similarly, or even less likely, to experience anxiety than the general population.12,13
It could be suggested that misdiagnosis coupled with such a significant diagnostic delay could often result in a lack of support and resources from health professionals for a number of years. One important issue that cannot be overlooked is that the types of changes involved in positive adaptation require clear support and validation from the environment. People living with chronic illness require significant others, peers and health professionals to acknowledge and validate the illness, in order for support and practical advice to be provided.14
The impact of PoTS on occupation
The PS versus PD occupational scores of ≤0.001 can be viewed as ‘very significant’15 and confirm that PoTS has a significant negative impact upon motivation, performance capacity and fatigue, across all three occupational domains.
Self-care
Within the sample, 60 participants (37.3%) required assistance from their partner to complete self-care activities, including washing, dressing and bathing, followed by assistance from family members at 29.2% (n=47). The PS versus PD scores revealed that performance capacity and fatigue were affected more than motivation. All three variables were, however, significantly affected at the <0.001 level.
There is evidence to suggest that support from an individual’s social network increases in response to a significant change in health needs or function.16 Thoits17 suggests that this can have a positive effect on the health of those living with chronic illness. However, having to rely on family to support basic activities such as self-care can lead to a sense of powerlessness and a loss of autonomy for some.18
Employment
There were 140 (57%) participants in some form of employment or education, while 72 participants (29.3%) were unable to work or study as a direct result of their symptoms.
One of the most significant effects on occupation in the current study was demonstrated in relation to employment and performance capacity. Participants were far less physically able to manage in employment in the PD versus PS. Participation in work is an important occupation, offering income, socialisation, daily rhythms and often, wellbeing and meaning in life.19
Education
A large proportion of 91 participants (44.8%) were educated/working at degree level, followed by 30 (14.8%) at A-level. The distribution of responses for masters, vocational training and GCSE was equal at 8.9%. While motivation to engage in education was significantly affected, it was marginally less affected than performance capacity and fatigue.
These statistics could reflect a number of possibilities. The first is that PoTS is more likely to affect younger people and younger people are more likely to be at a stage in their lives where education is considered an important, meaningful occupation. Second, education has been found to directly influence health behaviours and access to healthcare by a range of researchers.20,21 Therefore, it could be possible that educated young women are more likely to persist in their quest for answers as to why they have moved from being healthy and able to engage in a range of occupations to being limited by fatigue and reduced performance capacity.
Parenting
The PS/PD scores of 1.00 versus 4.00 in the parenting domain demonstrated a significant difference in performance capacity. According to Barnado’s,22 61% of British parents describe parenting as ‘fairly’ or ‘very difficult’ and these difficulties are increased for those who are living with a chronic illness, such as PoTS.23
Occupational therapists recognise that many adults living with a long-term condition have parenting responsibilities. The ways in which services for adults and families are designed, accessed and delivered should ensure that the parenting role is fully supported.22 Meeting the, often, conflicting needs of a variety of parents and families will be a challenge to occupational therapy services, nevertheless, providing personalised support to parents living with PoTS and their families is a goal worth attaining.
Social and recreational activity
The greatest observable effect within the current study can be found within social and recreational activity. The effect of fatigue upon this occupational domain was particularly marked (PS=5.00, PD=1.00). This investigation has touched upon functional limitations that can hinder social engagement and similar limitations have been found in other studies.24
Stout and Finlayson25 found that those living with a chronic health condition decrease their participation in social and leisure occupations due to the fact that such activities are viewed optional in comparison to activities, such as self-care, parenting and work. Stout and Finlayson go on to suggest that eliminating social activities may leave more energy for basic activities of daily living. However, quality of life may be negatively influenced as a consequence.25
Conclusion
Health is strongly influenced by having choice and control in everyday occupations, and this study demonstrates that those living with the symptoms of PoTS are restricted in those opportunities. People with PoTS experience significant disruption in relation to their motivation, performance capacity and fatigue, across all three occupational domains.
Occupational therapists have a vast skill
set, which is adaptable to multiple and complex problems, or minor coping difficulties. 26 This skill set could be utilised to facilitate people with PoTS to achieve a satisfying performance and balance of occupations that will support their health, wellbeing and social participation.
Conflict of interest
None declared.
Key messages
- Postural tachycardia syndrome (PoTS) has a significant negative impact upon motivation, performance capacity and fatigue, across all occupational domains
- Occupational therapists have the skill set to work with those who have PoTS in order to facilitate a balance of occupations that will support health, wellbeing and social participation.
References
1. McDonald C, Koshi S, Busner L, Kavi L, Newton J. Postural tachycardia syndrome is associated with significant symptoms and functional impairment predominantly affecting young women: a UK perspective. BMJ Open 2014;4:e004127. http://dx.doi.org/10.1136/bmjopen-2013-004127
2. Grubb BP. Postural tachycardia syndrome. Circulation 2008;117:21. http://dx.doi.org/10.1161/circulationaha.107.761643
3. Kavi L, Nuttall M, Low D et al. A profile of patients with postural tachycardia syndrome and their experience of healthcare in the UK. Br J Cardiol 2016;23:33. http://dx.doi:10.5837/bjc.2016.010
4. Wilcock A. An Occupational Perspective of Health. 2nd ed. Thorofare: Slack, 2006.
5. Hammell KW. Using qualitative evidence to inform theories of occupation. In: Hammell KW, Carpenter C, eds. Qualitative Research in Evidence-based Rehabilitation. Edinburgh: Churchill Livingstone, 2004; pp. 14–26. http://dx.doi.org/10.1016/B978-0-443-07231-4.50006-7
6. Yerxa E. An introduction to occupational science: a foundation for occupational therapy in the 21st century. Occup Ther Health Care 1990;6:1–17. http://dx.doi.org/10.1080/J003v06n04_04
7. Bagai K, Song Y, Ling JF et al. Sleep disturbances and diminished quality of life in postural tachycardia syndrome. J Clin Sleep Med 2011;7:204–10.
8. Benrud-Larson LM, Dewar MS, Sandroni P, Rummans T, Haythornthwaite J, Low P. Quality of life in patients with postural tachycardia syndrome. Mayo Clin Proc 2002;77:531–7. http://dx.doi.org/10.4065/77.6.531
9. Anderson JW, Lambert EA, Sari CI et al. Cognitive function, health-related quality of life, and symptoms of depression and anxiety sensitivity are impaired in patients with the postural orthostatic tachycardia syndrome (POTS). Front Physiol 25 June 2014. http://dx.doi.org/10.3389/fphys.2014.00230
10. Kielhofner G. A Model of Human Occupation. 4th ed. Baltimore: Williams & Wilkins, 2008.
11. Grubb B, Rowe P, Calkins H. Postural tachycardia, orthostatic intolerance and the chronic fatigue syndrome. In: Grubb B, Olshansky B, eds. Syncope: Mechanisms and Management. 2nd ed. Maiden: Blackwell/Future Press, 2005;pp. 225–44. http://dx.doi.org/10.1002/9780470994801.ch13
12. Khurana RK. Experimental induction of panic-like symptoms in patients with postural tachycardia syndrome. Clin Auton Res 2006;16:371–7. http://dx.doi.org/10.1007/s10286-006-0365-0
13. Masuki S, Eisenach JH, Johnson C et al. Excessive heart rate response to orthostatic stress in postural tachycardia syndrome is not caused by anxiety. J Appl Physiol 2007;102:896–903. http://dx.doi.org/10.1152/japplphysiol.00927.2006
14. Gray ML, Fossey EM. Illness experience and occupations of people with chronic fatigue syndrome. Aus J Occup Ther 2003;50:127–36. http://dx.doi.org/10.1046/j.1440-1630.2003.00336.x
15. Field A. Discovering Statistics Using IBM SPSS Statistics. 4th ed. London: Sage Publications, 2014.
16. Vassilev I, Rogers A, Blickem C et al. Social networks, the ‘work’ and work force of chronic illness self-management: a survey analysis of personal communities. PLoS ONE 2013;8. http://dx.doi.org/10.1371/journal.pone.0059723
17. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav 2011;52:145–61. http://dx.doi.org/10.1177/0022146510395592
18. Asbring P. Chronic illness – a disruption in life: identity-transformation among women with chronic fatigue syndrome and fibromyalgia. J Adv Nursing 2001;34:312–19. http://dx.doi.org/10.1046/j.1365-2648.2001.01767.x
19. van Campen C, Cardol M. When work and satisfaction with life do not go hand in hand: health barriers and personal resources in the participation of people with chronic physical disabilities. Soc Sci Med 2009;69:56–60. http://dx.doi.org/10.1016/j.socscimed.2009.04.014
20. Acheson D. Independent inquiry into inequalities in health report. London: The Stationery Office, 1998. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/265503/ih.pdf [accessed 14 July 2016].
21. The Marmot Review. Fair society, healthy lives. London: UCL Institute for Health Equity, 2010. Available from: http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot-review [accessed 14 July 2016].
22. Barnado’s. Parenting Support. Available at: http://www.barnardos.org.uk/what_we_do/our_work/parenting_supporting.htm [accessed 14 July 2016].
23. Commission for Social Care Inspection. Supporting disabled parents. A family or fragmented approach? London: Commission for Social Care Inspection, 2009. Available from: http://disabledparentsnetwork.org.uk/dpndocs/supporting-disabled-parents.pdf [accessed 14 July 2016].
24. Biordi DL, Nicholson NR. Social isolation. In: Larsen PD, Lubkin IM, eds. Chronic Illness: Impact and Interventions. 7th ed. Sudbury: Jones & Bartlett Publishers, 2009.
25. Stout K, Finlayson M. Fatigue management in chronic illness: assessment, treatment planning, and interventions. OT Practice 2011;16:16–19.
26. Hagedorn R. Tools for Practice in Occupational Therapy. Edinburgh: Churchill Livingstone, 2000.
