
Successful repair of tractional retinal detachment (TRD) in pediatric patients mainly due to retinopathy of prematurity (ROP) depends on the relief of traction on the retina caused by fibrotic vitreous. The fibrotic vitreous forms a thick membrane that tends to be circumferential, extending from the ridge to the anterior hyaloid face, including the ciliary body and lens.
AT A GLANCE
• Despite the availability of new technologies and devices for retinal surgery, the dissection of thick membranes is still a challenge.
• The author describes her technique for cutting and dissecting membranes in less traumatic way, without harming adjacent tissues.
• The use of a diathermy device for membranectomy in pediatric patients with TRD can simplify the vitrectomy procedure and allow the surgeon to perform a complete membranectomy with a higher index of successful attachment of the retina in stage 5 ROP.
Pediatric retina surgeons face a challenge when performing vitrectomy in preterm infants with stage 5 ROP because of the complexity of the detachment.1 In patients with anterior segment involvement with athalamia and synechiae, the surgical procedure includes lensectomy, complete capsulotomy, membranectomy, and vitrectomy, all performed in a closed three-port system from the anterior part of the eye, usually in
clear cornea.
Another challenge for the pediatric retina surgeon is trying to cut or dissect the retinal membranes because fibrotic retinal membranes in children are thick and hard. Moreover, in the attempt to remove them, it is possible to cause iatrogenic breaks that are very poorly tolerated in children and are rarely successfully repaired. This led us to seek a better way to cut and dissect membranes in a less traumatic way, without harming adjacent tissues. Our technique is described below.
SURGICAL TECHNIQUE
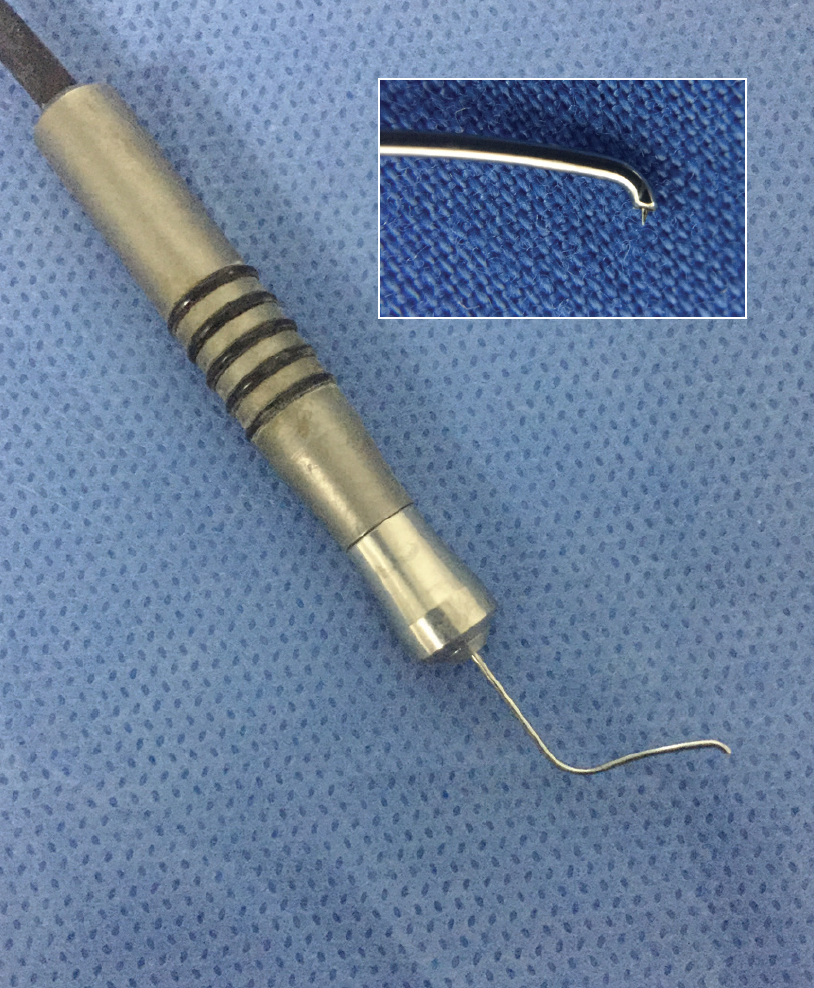
Figure 1. Capsulotomy “plug-on” tip for capsular phimosis. Inset: Close-up of the same device.
One instrument designed for another purpose but helpful in this situation is a 0.5-mm diathermy tip from Oertli called a capsulotomy “plug-on” tip for capsular phimosis (Figure 1). It is designed to cut the lens capsule with low power radiofrequency waves transmitted from the tip of an active incising electrode to make incisions in the tissue. The use of the low power radiofrequency energy and the high impedance contact prevents the active incising electrode from becoming hot and damaging the surrounding tissues.
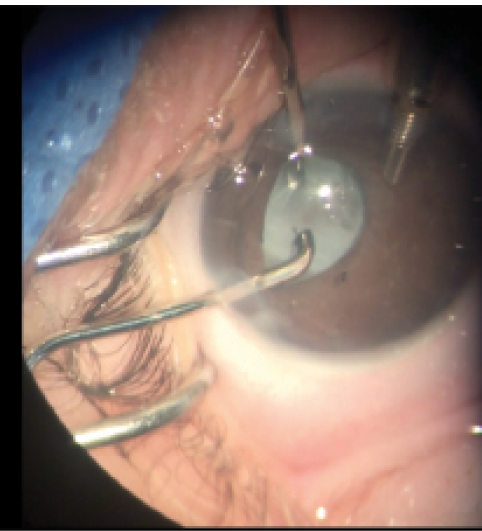
Figure 2. During use of the diathermy tip, air bubbles can appear in the anterior chamber, interfering with the surgeon’s vision.
We adapted this diathermy capsulotomy instrument to allow us to “melt” fibrotic membranes in pediatric eyes with ROP, sliding through the tissue without injuring the adjacent retina and relaxing the retinal traction. The tip of the instrument is pointed, allowing fine dissection of the membranes. The L-shaped tip facilitates access underneath the iris and ciliary processes to dissect the membrane toward the extreme periphery. The principal disadvantage of this technique is the appearance of air bubbles in the anterior chamber, which occur in every procedure and can interfere with the surgeon’s vision. When this occurs, an extra maneuver using viscoelastic to displace the bubbles is required (Figure 2).
CONCLUSION
In my surgical experience, the use of a diathermy device for membranectomy in pediatric patients with TRD can simplify the vitrectomy procedure. Furthermore, it allows me to perform a complete membranectomy with a higher index of successful attachment of the retina in stage 5 ROP. It also leads to shorter surgical times and allows safer dissection of membranes.
Despite the availability of new technologies and devices for retinal surgery, the dissection of thick membranes is still a challenge. Sometimes we can adapt tools that were designed for another purpose to improve or simplify our current techniques. n
1. Jandeck C, Kellner U, Foerster MH. Late retinal detachment in patients born prematurely: outcome of primary pars plana vitrectomy. Arch Ophthalmol. 2004;122(1):61-64.
Section Editor Albert Augustin, MD
• professor and chairman of the department of ophthalmology, Staedtisches Klinikum Karlsruhe, in Karlsruhe, Germany
Section Editor Ehab N. El-Rayes, MD, PhD
• professor of ophthalmology, Institute of Ophthalmology in Cairo, Egypt; vitreoretinal consultant, The Retina Clinic, in Cairo, Egypt
Section Editor, Masahito Ohji, MD
• professor and chairman of the department of ophthalmology, Shiga University of Medical Science, in Otsu, Shiga, Japan
Section Editor, Stanislao Rizzo, MD
• chair of the department of ophthalmology, University of Florence, in Florence, Italy
María Ana Martinez-Castellanos, MD
• pediatric retina surgeon, Asociación Para Evitar La Ceguera En Mexico, Mexico City
• financial interest: none acknowledged
• mamc@dr.com





















