- News
- lifestyle
- health-fitness
- health-news
- At Rs 30L, liver transplant only for rich
Trending
This story is from January 29, 2016
At Rs 30L, liver transplant only for rich
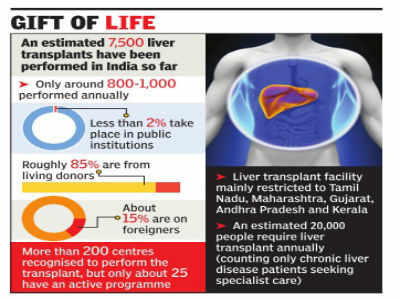
Less than 2% of liver transplants taking place in India happen in public institutions.
Key Highlights
• Less than 2% of liver transplants taking place in India happen in public institutions.
Less than 2% of liver transplants taking place in India happen in public institutions. This has meant that liver transplants, which cost Rs 20-30 lakh in most cases, are available only to the rich. This is not just an inequitable situation, but an unsustainable one, says a recently published paper reviewing the status of liver transplants in India.
"The future of liver transplantation in India should move toward a more accountable, equitable, and accessible form.We owe this to our citizens who have shown tremendous faith in us by volunteering to be living donors as well as consenting for deceased donation," wrote gastroenterological surgeon Dr Sanjay Nagral of Jaslok Hospital, Mumbai and two others who authored the paper published in the Journal of Clinical and Experimental Hepatology.
India's liver transplant programme might be flourishing but is marred by the lack of any mechanism for a registry or mandatory reporting of results too, the paper pointed out.
It is estimated that around 1015% of patients undergoing live donor liver transplants (LDLT) in India are from abroad. In some centres it is as high as 25%. Most are from the Middle East or from Pakistan, Sri Lanka, Bangladesh, and Myanmar. "We are not aware of any other country where the proportion of LDLTs for foreign patients is so high," stated the paper. It warned that other than regulatory issues such a difficulty in authenticating the paperwork and establishing relationship with donors, "excessive proliferation of LDLT for foreigners can potentially bring memories of the unfortunate period of organ trade that has haunted the history of transplantation in India".
The authors observed that there was a trend of even patients with treatable liver disease undergoing LDLT and called for caution in a situation of overwhelming dominance of live donors.
"We need to move from periodic laments and appeals to good sense to serious regulatory enforcement in an area where there is substantial international precedent," said the authors.
"The future of liver transplantation in India should move toward a more accountable, equitable, and accessible form.We owe this to our citizens who have shown tremendous faith in us by volunteering to be living donors as well as consenting for deceased donation," wrote gastroenterological surgeon Dr Sanjay Nagral of Jaslok Hospital, Mumbai and two others who authored the paper published in the Journal of Clinical and Experimental Hepatology.
India's liver transplant programme might be flourishing but is marred by the lack of any mechanism for a registry or mandatory reporting of results too, the paper pointed out.
It is estimated that around 1015% of patients undergoing live donor liver transplants (LDLT) in India are from abroad. In some centres it is as high as 25%. Most are from the Middle East or from Pakistan, Sri Lanka, Bangladesh, and Myanmar. "We are not aware of any other country where the proportion of LDLTs for foreign patients is so high," stated the paper. It warned that other than regulatory issues such a difficulty in authenticating the paperwork and establishing relationship with donors, "excessive proliferation of LDLT for foreigners can potentially bring memories of the unfortunate period of organ trade that has haunted the history of transplantation in India".
In India 85% of liver transplants are from live donors. The rules permit live donation from those who are not first degree relatives only with special permission from the state transplant authority. Though precise data is unavailable, a substantial number of donors are family members beyond first-degree relatives or even unrelated donors, noted the paper, cautioning that in the context of donor problems not being uncommon, it could lead to a hazardous situation.
The authors observed that there was a trend of even patients with treatable liver disease undergoing LDLT and called for caution in a situation of overwhelming dominance of live donors.
"We need to move from periodic laments and appeals to good sense to serious regulatory enforcement in an area where there is substantial international precedent," said the authors.
End of Article
FOLLOW US ON SOCIAL MEDIA