It's crucial to know the most common artifacts in MRI and try to overcome them, as well as to recognize the diagnostic pitfalls they can mimic, according to researchers from Portugal. They also emphasize that these artifacts can have clinical utility and may assist with a diagnosis.
Artifacts, which are structures that are not anatomically present but are visible in a MRI examination, can have many causes and consequences. In order to reduce their impact and obtain the best possible images, it's necessary to learn about them, explained Dr. Ana Luísa Cipriano Duarte, a radiologist at Serviço Nacional de Saúde, Hospital do Espírito Santo de Évora in Évora, and colleagues. They emphasize that radiologists must be able to recognize them in order to avoid diagnostic pitfalls and try to prevent them from happening.
MRI artifacts can be classified by their basic principles: those dependent on physiological processes (breathing, heartbeat, flow in vessels), movement artifacts, flow artifacts, those inherent to the physical processes used in MRI, chemical shift (first and second type), aliasing, magnetic susceptibility artifacts, those inherent to the software and hardware of an MRI system, cross-talk artifacts, and zipper artifacts.
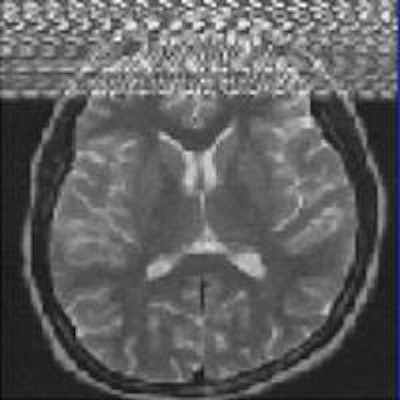
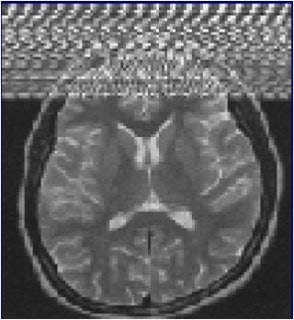 Zipper artifacts, when a radiofrequency (RF) wave interferes with the MRI unit, may occur if a medical device that is not RF-shielded is placed inside the magnet room. Other causes are blinking light bulbs, the examination room door not being tightly closed, and drilling work nearby. Image courtesy of IGK Kusumasuganda, mriforyou.blogspot.co.uk.
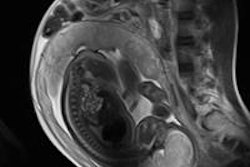
Zipper artifacts, when a radiofrequency (RF) wave interferes with the MRI unit, may occur if a medical device that is not RF-shielded is placed inside the magnet room. Other causes are blinking light bulbs, the examination room door not being tightly closed, and drilling work nearby. Image courtesy of IGK Kusumasuganda, mriforyou.blogspot.co.uk.Motion artifacts occur in the phase-encoding axis of the k-space encoding, which usually happens in the vertical axis of the MR image, and this encoding direction of the k-space is considered "slow" and can even take some minutes, they stated in an e-poster at ECR 2015. As the image is being encoded or acquired, motion can occur and different timings are recorded, and hence the final image will not have clear borders and "ghost images" or even spatial blurring occur in the phase-encoding axis of the image.
"Random motion artifacts produce a blurry and noisy image, mainly in the phase-encoding direction, while periodic motion artifacts create ghost images in the phase-encoding direction (e.g., the pulsatility of the arteries, pulsatility artifact)," the authors noted.
To help overcome random motion artifacts, the patient should be made as comfortable as possible. Be responsive to the patient's doubts and anxiety and try to inform him or her about the examination steps and the importance of being still at certain times, and administer antispasmodic medication like butylscopolamine bromide if you are facing peristaltic motion, they recommend.
For periodic motion artifacts (breathing, heartbeat), use faster sequences that can be obtained in inspiratory apnea, while respiratory or cardiac gating increases the acquisition time and can be useful. With respiratory-ordered phase encoding (ROPE), each line of the phase-encoding direction of the k-space is obtained according to a particular moment of the respiratory cycle, but this is only effective in patients that have regular respiratory cycles, continued Duarte and her colleagues. Navigator echo gating involved placing a navigator in the imaged diaphragm to determine the diaphragmatic position, and the timing of the acquisition is adjusted so that data are acquired only during a specific range of diaphragmatic motion.
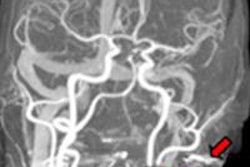
Gradient echo (GRE) sequences are much more susceptible to flow artifacts than are spin-echo (SE) sequences, they pointed out. In SE sequences, the flow usually appears dark, producing no signal, because the flowing blood that is exposed to the 90° excitation pulse moves out of the imaging section before the refocusing 180° pulse is applied, while the blood that moved into that section was never exposed to the excitation pulse.
"In GRE imaging, the in-flow effect produces the bright-blood phenomenon. The spins of the protons in GRE sequences 'need' multiple radio-frequency (RF) pulses to achieve a steady state - i.e., a state where longitudinal and transverse magnetization are constant in order to obtain the image," Duarte et al noted. "As the blood is in constant circulation, its spins do not receive these multiple pulses to achieve a steady state. In fact, they receive a RF pulse immediately before the image acquisition, so they will emit signal and will appear in the image with a bright and intense signal."
Two techniques can be used to attenuate them:
Saturation bands. These are applied before the slice that is being acquired. All spins are saturated in the slice immediately upstream to the selected slice to be imaged, so when the blood is circulating into the selected slice, its spins will already be saturated, and when the image is acquired, they will produce no signal.
Gradient moment "nulling." Several additional motion-compensating gradient pulses can be applied to try to correct the difference of phase between the flowing spins (in the blood, for example) and the static spins (those in the surrounding tissues) whilst the image is being acquired.
To solve chemical-shift artifacts, increase the receiver bandwidth (which will worsen the signal-to-noise ratio), reduce the matrix size (which will decrease the spatial resolution), or suppress the fat-frequency signal, they suggested.
Aliasing, or a "wrap-around" artifact, happens because of an under-sampling of the k-space, and it can occur in the frequency-encoding or phase-encoding direction. It is actually only an issue in the phase-encoding direction, because this encoding is much slower and the oversampling of the frequency encoding can be done while the phase encoding is still being done.
Doubling the number of lines acquired in the phase-encoding direction increases the acquisition time and increases the risk of motion artifacts, the authors wrote. Other options are to use dedicated coils that will attenuate the signal received outside the field-of-view (FOV), increase the FOV (decreasing spatial resolution), swap the phase-encoding and frequency-encoding axis so that the phase-encoding occurs in the lesser axis of the image, and apply saturation bands around the desired FOV.
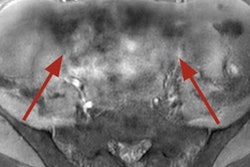
"Magnetic susceptibility artifacts have clinical and diagnostic utility," they explained. "In the detection of hematomas or old hemorrhagic focus, they are extremely useful in these situations: blood breakdown products (like hemosiderin) cause susceptibility artifacts that are responsible for loss of signal with 'blooming effect' in T2* GRE sequences."
Zipper artifacts are related to the contamination of electromagnetic energy in the MRI suite. MRI suites should be isolated in order to avoid external interference from other sources of RF or from electronic equipment like radios and cellphones that emit electromagnetic signal and can cause interference. Contamination usually happens because of equipment that is wrongly brought into the MRI suite, and the artifact disappears as soon as this external source of frequency is removed from the MRI suite. If the artifact persists, it probably means the isolation of the MRI suite has been compromised.
To learn more about these artifacts, the authors recommend this e-chapter by Denis Hoa.