A Call for Leadership and Reflection
This is Bob Harrington from Stanford University. I'm at the American College of Cardiology (ACC) meetings in San Diego and wanted to take a few minutes to reflect on news that might be of interest to the broader cardiology community and some of the things that we have learned here over the past few days. I will break this into three or four categories.
San Diego is a fantastic place to have a meeting. If you didn't attend, I'm sorry you missed it. It has been absolutely beautiful here. The weather has allowed us to extend the educational opportunities into different venues. This morning, I conducted a live journal club with a few colleagues, Dipti Itchhaporia and Harlan Krumholz, in the outdoor amphitheater overlooking the bay. It was a great location, and we had a great discussion on the PROMISE trial.[1,2] I will come back to that.
In the opening session, Pat O'Gara, the president of the ACC, talked about the opportunities and challenges in global cardiology; the threats we face from constrained graduate medical education funding and declining public research funds but also the tremendous opportunities that we have through wearable technologies and the use of big-data analytics to better understand what we are doing. Pat presented both a realistic view of the challenges but also some real opportunities for us to think about. He wrapped all of that in a call for leadership from the cardiovascular community, not just in how we think about what is going on in cardiovascular medicine but how we think about some of the broader issues in healthcare.
As part of the opening ceremony, my friend and colleague from Stanford University, Abraham Verghese, gave the Simon Dack lecture. You know it's something special when you are in the opening sessions at a scientific meeting and the speaker, without slides or PowerPoint or any of the things we are used to seeing at these meetings, reads us a poem by e.e. cummings, "Carry Your Heart." It was an inspirational moment for many of us in the audience to think about what cardiovascular medicine is about.
Yes, it's about science. Yes, it's about data. Yes, it's about all of the things that we talk about at a meeting like this. But what it's really about is connecting to one another and to our patients and listening to our patients. He talked a lot about how such barriers as the electronic health record might get in the way of those relationships. He caused many of us to think. I have been here at the meeting for several days, and at least once an hour, somebody sees me in the hallway and says, "Did you go to the opening ceremony? What did you think?" It was a different aspect for our meeting, and it resonated with our members here in the ACC who are feeling tremendous pressures in the practice of medicine. It was a good reminder of why we do what we do.
Hot Science: PROMISE and PEGASUS
The last thing I want to bring up are two of the hot pieces of science that I heard at these meetings. I happened to be on the panel Saturday morning for the late-breaking clinical trials where PROMISE and PEGASUS[3,4] were presented. By way of full disclosure, I was director of the Duke Clinic Research Institute at the time the PROMISE trial started, but I have had nothing to do with the oversight of the trial and have been gone from Duke for a couple of years. For the PEGASUS trial, I was one of the principal investigators, along with Lars Wallentin, of the earlier PLATO trial,[5] which we reported out in 2009. I have had nothing to do with the oversight of the PEGASUS trial.
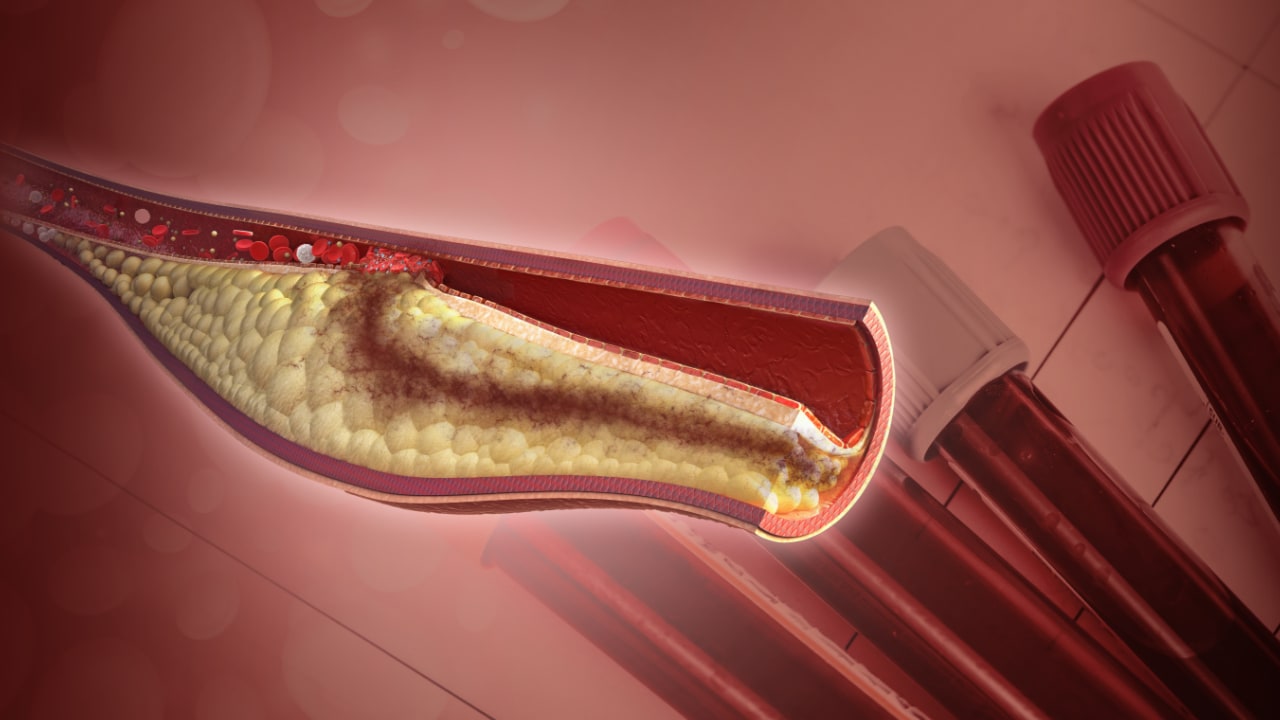
Let's start with PROMISE, and as a corollary to PROMISE, I will pull in some of the findings from SCOT-HEART.[6,7] PROMISE was a very interesting trial led by Pam Douglas and Udo Hoffmann, trying to understand the strategy of assessment in the workup of patients with low-risk chest pain. A large number of people come to American emergency rooms for the evaluation of acute chest pain, and we don't have a great sense of how we should evaluate them. We do it with history, physical examination, electrocardiogram, and biomarkers, etc., but for many of these patients, there is uncertainty about the optimal testing strategy. Is it a functional test, such as electrocardiogram testing, stress testing, echo stress testing, or nuclear stress testing? Or is it an anatomic assessment, using CT angiography, for example?
This was a large randomized trial of 10,000 patients to try to compare one strategy with the other. What did we learn? We learned that in a well-cared-for group of patients, these event rates are actually a lot lower than had been anticipated on the basis of available pretrial data. That was one of the reasons that no one strategy emerged as superior over another; the event rates were insufficient for that determination. With respect to CT angiography, as an interventional cardiologist, one thing I found interesting was that we learned, as a secondary endpoint, that the likelihood of having obstructive coronary disease at the time of cardiac catheterization is much higher, not surprisingly, if the patient has already had a CT angiography study.
Why might that finding be valuable? It potentially can help us hone in on the group of patients who need to be taken to the cath lab, who have a likelihood of disease, and whose disease is likely to be amenable to revascularization. The entire question of whether we even need to revascularize patients as part of this catheterization strategy is being tested in the ISCHEMIA trial,[8] which is led by David Maron and Judy Hochman, looking at a slightly higher-risk group of patients with moderate to severe ischemia. So, we will have more to come on that front.
Top Take-Home Messages
The SCOT-HEART study looked at the addition of CT angiography to medical therapy in Scotland in patients with chest pain. That study suggested that there was incremental value to CT angiography; in particular, as with the PROMISE trial, for gaining an understanding of the presence of obstructive disease before getting to the cath lab. All in all, these will be good data for the writers of guidelines and appropriate use criteria.
Finally, from the PEGASUS trial, I learned a couple of things that are worthwhile to think about. In this trial, the adenosine diphosphate (ADP) receptor blocker ticagrelor, which is approved for use in the acute coronary syndrome setting, was used much later than the acute care setting (beyond 1 year after myocardial infarction) in patients who had other high-risk factors. We learned that the addition of ticagrelor to standard therapy offered an incremental benefit over placebo. One important piece of information from this study is that risk continues to accrue over time. We knew that, but continued validation and attention to the need for aggressive secondary prevention are important.
A second important take-home message is that a much lower dose of ticagrelor was studied in this trial than that used in the PLATO trial. The PEGASUS investigators included the PLATO dose of 90 mg twice daily but also included a second active treatment arm in which patients received 60 mg twice daily, which provided comparable ischemic benefits but less bleeding compared with the higher dose. This is perhaps not surprising, but it tells us that we may be able to better personalize therapy over time to try to reduce the risk of bleeding. This is an important observation. We are going to have to consider this as we think about prescribing long-term antiplatelet therapy.
One more finding from PEGASUS pleased me as a PLATO investigator. In PLATO, the treatment effect looked different. It went in the other direction in North America and particularly in the United States relative to the other global regions. The good news coming out of PEGASUS is that the point estimates of benefit for all regions line up with the overall trial results. This is an important observation and perhaps removes some of the uncertainties about the benefit of ticagrelor in the United States based on the PLATO trial.
That is a quick run-through of some of the things I have learned here in San Diego. I hope that you have found this interesting and informative. Thanks for listening.
© 2015 WebMD, LLC
Cite this: Bob Harrington's ACC: Poetry, PROMISE, and PEGASUS - Medscape - Mar 24, 2015.











Comments