Abstract and Introduction
Abstract
Background Protease-activated receptor 1 antagonism with vorapaxar represents a novel strategy for platelet inhibition. In TRACER, vorapaxar was compared with placebo plus standard of care among 12,944 patients with non–ST-segment elevation acute coronary syndromes. We anticipated that most patients would have received clopidogrel as part of standard care. We investigated the modification of vorapaxar's effect associated with clopidogrel use over time.
Methods The marginal structural model method was used to estimate causal modification of vorapaxar effect by use of clopidogrel over time. The primary outcomes were the composite of cardiovascular death, myocardial infarction, or stroke and Global Use of Strategies to Open Occluded Coronary Arteries moderate or severe bleeding. The event accrual period excluded the time during which clopidogrel was clinically warranted.
Results Among 12,887 patients who received study medication, 11,117 (86.3%) received clopidogrel before randomization, of whom 38.5% stopped later in the trial (median time to stoppage 200 days with placebo; interquartile range [IQR] 14–367) (186 days with vorapaxar; IQR 17–366). In total, 1,770 (13.7%) patients were not on clopidogrel at randomization, of whom 47.8% started afterward (median time to start 2 days; IQR 2–4). During the period of event accrual, vorapaxar was associated with a 26% reduction in the composite of cardiovascular death, myocardial infarction, or stroke when used with clopidogrel (hazard ratio [HR] 0.74; 95% CI 0.60–0.91) and a 24% reduction when used without clopidogrel (HR 0.76; 95% CI 0.56–1.02) (interaction; P = .89). The hazard of Global Use of Strategies to Open Occluded Coronary Arteries bleeding with vorapaxar was not significantly different without clopidogrel (HR 1.33; 95% CI 0.81–2.20) or with clopidogrel (HR 1.09; 95% CI 0.76–1.56) (interaction; P = .53).
Conclusions We observed no interaction between vorapaxar and clopidogrel after non–ST-segment elevation acute coronary syndromes on efficacy or safety outcomes, supporting a complementary role of protease-activated receptor 1 and P2Y12 antagonism.
Introduction
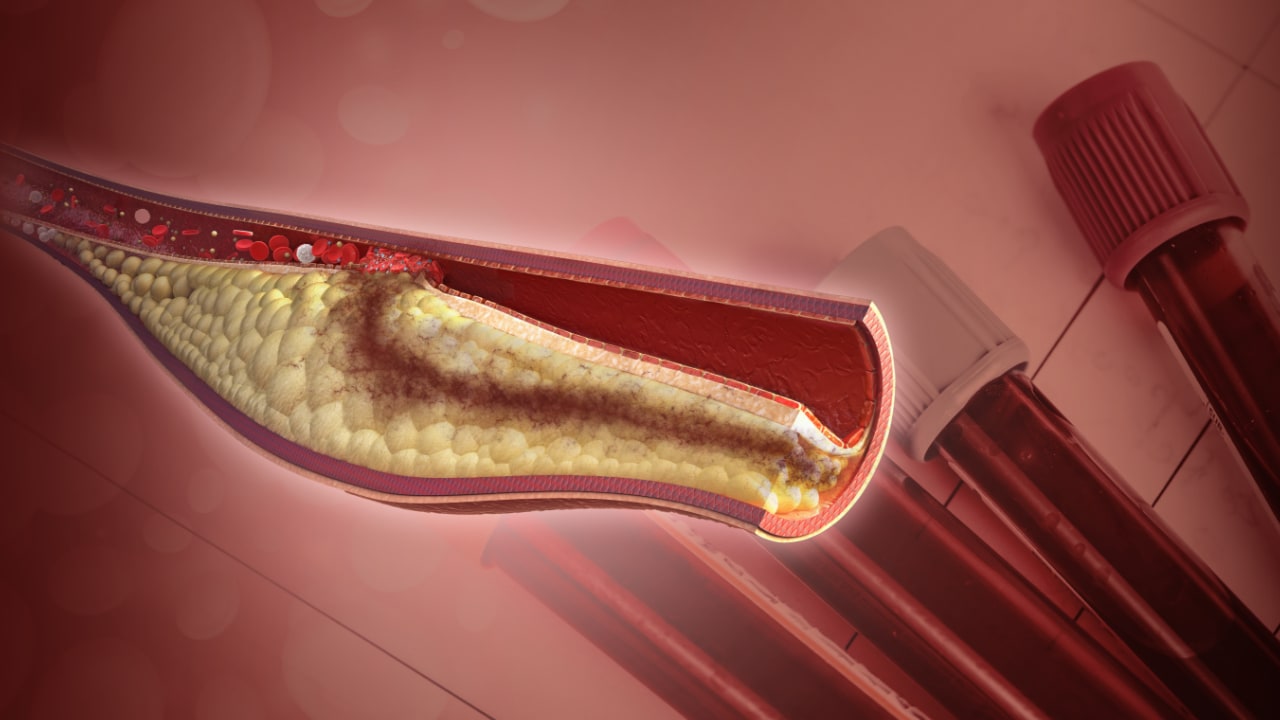
Vorapaxar is an oral, selective, protease-activated receptor 1 (PAR-1) antagonist. Thrombin-induced platelet activation is mediated by PARs and is considered to be the main thrombin receptor in humans.[1] Vorapaxar administration results in potent inhibition of PAR-1–mediated platelet aggregation.[1]
The TRACER trial was a large, international, phase III clinical trial that evaluated the efficacy and safety of vorapaxar compared with placebo in patients presenting with non–ST-segment elevation acute coronary syndromes (NSTE ACS) who were treated with standard of care.[2] The TRACER trial did not meet its primary objective, with a nonstatistically significant 8% reduction in the composite of cardiovascular death, myocardial infarction (MI), stroke, coronary ischemia with hospitalization, or urgent coronary revascularization.[2] A nominally significant 11% reduction in the key secondary end point of cardiovascular death, MI, or stroke was observed with vorapaxar and was driven by a reduction in MI. Vorapaxar significantly increased the risk of major bleeding. In the TRA 2P–TIMI 50 study, a large phase III trial of vorapaxar for secondary prevention of atherothrombosis, vorapaxar also significantly reduced cardiovascular death, MI, and stroke.[3]
As part of the standard of care in TRACER, most patients were treated with dual antiplatelet therapy, with clopidogrel as the most commonly used P2Y12 inhibitor. We designed this analysis to assess whether the observed effects of vorapaxar in TRACER were modified by concomitant exposure to clopidogrel. Assessing interaction between chronic antithrombotic therapies presents several analytical challenges, and thus, we have implemented the marginal structural model (MSM) method, aiming to control for time-dependent confounders.
Am Heart J. 2014;168(6):869-877. © 2014 Mosby, Inc.
Copyright © Mosby-Year Book, Inc. All rights reserved.