I was almost run over by a gurney being pushed by a fast-moving Emergency Medical Technician. He thrust the patient's chart at me. "Doc, you'll want to check this lady out quick. She's not looking good."
The first thing I noticed was the color of her skin. Its greyish green hue signaled death's approach. She had a nasal trumpet stuffed in her tiny nose and the quietest gurgle rattled around deep inside the tube. The only movement I could discern was a flaring of the tube-filled nostril, as if she were trying to expand it away from the large plastic invader.
She was 95, a tiny withered woman with leathery skin stretched loosely over her face. She was delirious and every few minutes mumbled incomprehensibly. She breathed fast and then slow, then fast again, as if she couldn't remember how to choreograph basic physiologic functions. Her vital signs were dismal.
As the ICU attending, I wondered if I should prepare to intubate her. I asked the nurse to collect the required equipment and medications. Then I saw it -- in the back of the chart, behind the EKGs, lab reports, and recent hospital discharge summary --the bright pink of a POLST form.
A Physician Order for Life-Sustaining Treatment is a legal document that is signed by a physician or nurse practitioner, outlining the type of medical care her patient should be given if critically ill. Unlike a DNR, which is active only for a particular hospitalization, the POLST is valid anywhere and anytime, unless the patient rips it up. Emergency personnel in most states must honor it, whether the patient is at home, in transit, or in the hospital.
This one was checked "Do Not Attempt Resuscitation (DNAR) in the event of a cardiac arrest." "Comfort Measures Only" (CMO) was identified as acceptable medical treatment in section B. In short, this patient had specified that treatments should be aimed at treating symptoms, without attempting to prolong her life. Chest compressions, cardiac shocks, and breathing machines were out--- treatments for shortness of breath or pain, for example, were in.
This directive is rare, but requires urgent recognition. The POLST form was invented in Oregon in 1991, and has slowly gained recognition in other states since. Until recently, the bright pink forms were almost impossible to find around the hospital, and only patients who had received consultation from the Palliative Care service were provided access to them. Over the past few months, I have occasionally spotted them on the wards. Unfortunately, they remain seldom used.
Anyone can get the full court press treatment of life-prolongation. It is the default approach that we take with everyone. But if a patient instead decides that when the time comes, she wants to die a natural death and avoid life-support machines, she must have a physician sign a POLST form in order to protect this wish. And so doctors and first responders must be compulsive about looking for this bright pink form.
I needed to turn this impending Code Blue into a Code POLST.
The official State of California Emergency Medical Services page emphasizes the importance of the POLST form, providing instructions and links. And yet this patient's POLST form had gotten lost in a pile of papers. Except for a chance sighting, I too would have missed it, in all of its pinkness.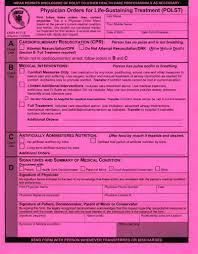
This phenomenon is unfortunately all too common. My friend's son, a rookie EMT, and himself savvy about the importance of this form, told me that he had been surprised by his squad's lack of familiarity with it. When he explained to them how important it had been for his own grandmother, on whose fridge it was tacked for months before her peaceful death at home, their initial confusion gave way to an "of course" moment. Anyone who rides around a city assisting its sickest people has seen too many cases of traumatic and futile resuscitation to fail to grasp its relevance.
So why aren't EMTs better trained on this issue? Unfortunately, it represents a larger cultural problem. Paragraph nine of the state EMS web page states that if a POLST form cannot be found, the EMT is directed to "err on the side of the patient... and provide life support."
To me this is a non sequitur. Of course EMTs should try to prolong life if they don't know what the patient's wishes are. As an ICU attending, I do the same, frequently and with vigor.
Rather, my concern is about the cultural implications of this statement. All health care workers -- whether EMTs, ICU doctors, or hospice nurses -- are trained to be "on the side of the patient." When I midwife death, I care just as much about my patient as I do when trying to save her life. This language points to a greater cultural issue: that allowing a chosen death is a failure, is morally wrong, and demonstrates an abandonment of the patient and our vocation.
I'm not singling out EMTs, nursing homes, or doctors. All health care workers, particularly those of us on the front lines of care, need to recognize and protect those patients who have chosen to allow a natural death. Being first responders, we set the course of that patient's particular interaction with the healthcare system, a course that is very hard to change once initiated.
In my eyes, that bright pink form is gold. Let's make sure that first responders like myself treat it accordingly.
